What is arthritis of the shoulder (Glenohumeral Arthritis)?
The glenohumeral joint, commonly called the shoulder joint, is a ball-and-socket joint made up of the top, rounded portion of the humerus (the ball) and the dish-shaped part of the outer edge of the scapula, called the glenoid.
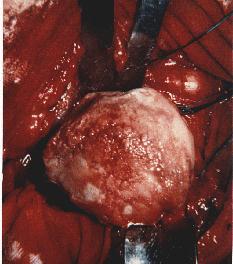
Arthritis of the shoulder, or glenohumeral arthritis, affects the glenohumeral cartilage in the shoulder. Cartilage is a slick elastic connective tissue that provides a smooth gliding surface enabling efficient joint motion.
 What are causes of arthritis of the shoulder?
What are causes of arthritis of the shoulder?
Destruction of the glenohumeral cartilage occurs as a result from:
- Osteoarthritis
- Rheumatoid arthritis
- Postraumatic arthritis
- Rotator cuff tears
- A history of shoulder fractures or dislocations
Repetitive overhead lifting, such as that done by weightlifters or construction workers who reach overhead, can increase the incidence of the disease. People with a history of instability and dislocations are especially vulnerable to develop arthritis. A history of a chronic massive rotator cuff tear can result in an aggressive destruction of the glenohumeral joint.
What are the symptoms of arthritis of the shoulder?
One of the first signs that a person may have glenohumeral arthritis is pain and tenderness in the shoulder area and upper arm. Patients often describe a knife-like sharp pain radiating from the back of the shoulder to the front. Sometimes patients will report pain in the forearm. Loss of motion is common, especially external rotation. Compression of the joint, which may occur when picking up an object away from the body, will cause pain. Patients with arthritis of the shoulder will have trouble doing everyday activities, like reaching overhead, washing their back, or sleeping on their affected side.
How is glenohumeral arthritis diagnosed?
 Most of the information to diagnose arthritis comes from the patient’s symptoms. On physical exam, the physician will often notice decreased motion, especially external rotation. Crepitus, or the sensation of grating, can be felt or heard with motion. Patients will often describe a knife-like pain when they attempt to lift objects away from their body. Occasionally, an injection directly into the glenohumeral joint (not into the subacromial space, which is done for rotator cuff problems) with is given. This should relieve symptoms at least temporarily if arthritis is present.
Most of the information to diagnose arthritis comes from the patient’s symptoms. On physical exam, the physician will often notice decreased motion, especially external rotation. Crepitus, or the sensation of grating, can be felt or heard with motion. Patients will often describe a knife-like pain when they attempt to lift objects away from their body. Occasionally, an injection directly into the glenohumeral joint (not into the subacromial space, which is done for rotator cuff problems) with is given. This should relieve symptoms at least temporarily if arthritis is present.
X-rays are obtained to evaluate for joint space narrowing and spur formation. It is imperative that an axillary x-ray is obtained to determine if there is bone loss in the posterior glenoid. If there is too much bone loss some surgical options are lost because the glenoid (the cup) will not support a prosthesis. MRI and CT scans are generally required to evaluate arthritis. An MRI is obtained if there is a question to the integrity of the rotator cuff and a CT scan may be obtained if the amount of bone loss must be further evaluated.
What is the treatment of shoulder arthritis?
Treatment is initially conservative. Anti-inflammatory medication (Advil, ibuprofen, naproxen), ice, and avoidance of aggravating activities are first attempted. A corticosteroid injection into the glenohumeral joint may be tried. Most studies have shown approximately 6 to 8 weeks of relief from these injections. Up to 4 injections per year (every 3 months) can be safely given with no detriment to your shoulder.  When a patient with arthritis loses motion, their shoulder becomes more painful. Therefore, an aggressive passive physical therapy program often results in significant pain relief.
When a patient with arthritis loses motion, their shoulder becomes more painful. Therefore, an aggressive passive physical therapy program often results in significant pain relief.
At this time, we have no way to replace worn out cartilage. Therefore, if all conservative options have been exhausted, the next treatment is usually a total shoulder replacement. The ball portion of the joint is replaced with an alloy metal ball attached to a metal stem to hold the ball in position. The glenoid, or cup, is replaced with a metal tray and a special plastic dish. The plastic is called ultra-high molecular weight polyethylene which is a high-tech low friction material that becomes the new bearing surface, or joint. Some centers hold the plastic dish in the shoulder with cement. We have found that our results are better with longer survival when the glenoid is replaced with a metal tray that is “press-fit” (no cement) into place.
At times there are reasons that only the ball portion of the shoulder can be replaced. A glenoid replacement cannot be performed if there is a significant amount of bone loss. If this is the case, a hemiarthroplasty (replacement of the ball only) is performed. Occasionally, only the ball portion is damaged (i.e. after a fracture) and the surgeon may elect to replace only the ball.
Shoulder Resurfacing
 Another procedure that is available for glenohumeral arthritis is a resurfacing procedure. The potential advantages of humeral resurfacing, as compared with conventional shoulder arthroplasty, are: (1) no osteotomy is performed (and thus the head-shaft angle does not have to be addressed); (2) minimal bone resection; (3) a short operative time; (4) a low prevalence of humeral periprosthetic fractures; and (5) ease of revision to a conventional total shoulder replacement, if needed. Outcomes of surface replacement arthroplasty have been comparable with those of arthroplasties with a stemmed prosthesis in numerous short and mid-term follow-up studies.
Another procedure that is available for glenohumeral arthritis is a resurfacing procedure. The potential advantages of humeral resurfacing, as compared with conventional shoulder arthroplasty, are: (1) no osteotomy is performed (and thus the head-shaft angle does not have to be addressed); (2) minimal bone resection; (3) a short operative time; (4) a low prevalence of humeral periprosthetic fractures; and (5) ease of revision to a conventional total shoulder replacement, if needed. Outcomes of surface replacement arthroplasty have been comparable with those of arthroplasties with a stemmed prosthesis in numerous short and mid-term follow-up studies.



