What is the knee meniscus?
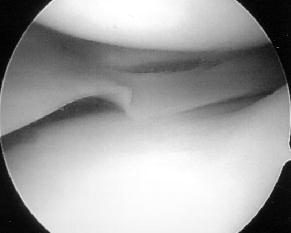
 There are two menisci in your knee: each is a crescent-shaped disc that rests between the thigh bone (femur) and the shin bone (tibia). The menisci are made of tough cartilage and conform to the surfaces of the bones upon which they rest. The lateral meniscus rests on the lateral tibial plateau. The other meniscus, the medial meniscus, rests on the medial tibial plateau. These menisci function to distribute your body weight across the knee joint. Without the meniscus present, the weight of your body would be unevenly applied to the bones of your legs (the femur and tibia). This uneven weight distribution would cause excessive forces in specific areas of bone leading to early damage of these areas. Therefore, the function of menisci is critical to the health of your knee. The menisci are nourished by small blood vessels, but also have a large area in the center of the meniscus that has no direct blood supply (it is avascular). This lack of circulation presents a problem when there is an injury to the meniscus, as the avascular areas tend not to heal.
There are two menisci in your knee: each is a crescent-shaped disc that rests between the thigh bone (femur) and the shin bone (tibia). The menisci are made of tough cartilage and conform to the surfaces of the bones upon which they rest. The lateral meniscus rests on the lateral tibial plateau. The other meniscus, the medial meniscus, rests on the medial tibial plateau. These menisci function to distribute your body weight across the knee joint. Without the meniscus present, the weight of your body would be unevenly applied to the bones of your legs (the femur and tibia). This uneven weight distribution would cause excessive forces in specific areas of bone leading to early damage of these areas. Therefore, the function of menisci is critical to the health of your knee. The menisci are nourished by small blood vessels, but also have a large area in the center of the meniscus that has no direct blood supply (it is avascular). This lack of circulation presents a problem when there is an injury to the meniscus, as the avascular areas tend not to heal.
What causes a torn meniscus?
Meniscus tears can occur during rotating movements while bearing weight, such as when twisting the upper leg while the foot stays in one place during sports and other activities. Tears can be minor, with the meniscus staying connected to the knee, or major, with the meniscus barely attached to the knee by a cartilage thread. As we age, normal degenerative changes can occur to the meniscus. It is imperative that the physician distinguish normal age related changes from a torn meniscus as the cause of the symptoms.
What are the symptoms of a torn meniscus?
Generally, when people injure a meniscus, they experience mechanical-type symptoms. These symptoms include a sensation of locking, catching, and giving way of the knee. Severe pain may occur if a fragment of the meniscus catches between the femur and tibia. Swelling may occur soon after the injury if blood vessels are disrupted, or swelling may occur several hours later if the joint fills with fluid produced by the joint lining (synovium) as a result of inflammation. Symptoms of meniscal injury may disappear on their own but frequently, symptoms persist or return and require treatment.
It is important for the physician to distinguish the mechanical symptoms of a meniscus tear from the more diffuse symptoms of arthritis (DJD – ‘degenerative joint disease’). Patients that have DJD will more commonly state that they have pain the morning (morning stiffness), pain and stiffness as they begin an activity (start-up pain), and develop a dull toothache-type pain as they walk for a distance.
How is a torn meniscus diagnosed?
The patient’s history (mechanical complaints) can usually provide the physician with enough information to diagnose a torn meniscus. The physician should perform a careful exam to look for findings specific to a meniscus tear. Tenderness along the joint line of the painful side of the knee (medial or lateral) is consistent with both a torn meniscus and with arthritis. If the patient has a positive McMurray test (moving the knee in a position to place pressure between the femur and tibia to compress the torn meniscus) this will elicit pain in a patient that has a meniscus tear. Swelling in the knee is generally a non-specific finding, simply suggesting that the knee is aggravated. X-rays should be obtained to evaluate the amount of arthritis in the knee. A torn meniscus will not appear on an x-ray and a knee with significant arthritis can still have a symptomatic meniscus tear. If the physician is unsure that a meniscus tear is present, he/she will obtain an MRI. An MRI is sensitive for the soft tissues in the knee (meniscus, ligaments, ACL) and is positive when fluid (or a bright line) appears within the meniscus. It is normal for menisci to have age related changes as we get older and the physician should carefully correlate the degree of MRI findings with the patient’s symptoms.
What is the treatment for a torn meniscus?
 If the torn meniscus is recent, often conservative treatment (anti-inflammatories, ice, rest) for 2-4 weeks will result in a decrease in symptoms. Although a meniscus will generally not heal on its own, it can essentially scar down to a new stable position and stop causing symptoms. Occasionally, a corticosteroid injection will also be given to decrease inflammation and speed symptom improvement.
If the torn meniscus is recent, often conservative treatment (anti-inflammatories, ice, rest) for 2-4 weeks will result in a decrease in symptoms. Although a meniscus will generally not heal on its own, it can essentially scar down to a new stable position and stop causing symptoms. Occasionally, a corticosteroid injection will also be given to decrease inflammation and speed symptom improvement.
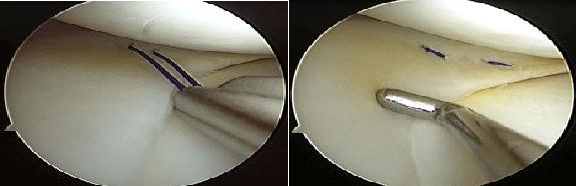
If the knee continues to experience mechanical symptoms (locking, catching, giving way) then usually a knee arthroscopy is required. Two small incisions are made on the front of the knee and, using a camera and small instruments, the torn portion of the meniscus is removed. Only the torn portion is removed, as the remaining meniscus serves the important function of load distribution and knee stability. The weight bearing function of the meniscus is never the same again after a meniscus tear, as the torn portion of the meniscus no longer performs this role as well. The torn portion will continue to cause symptoms as long as it is present.
What type of recovery can I expect after a meniscectomy?
The surgery typically takes 45 minutes to one hour, and can be performed while the patient is awake or asleep, depending on the patient’s preference. The patient goes home the same day, and is discharged with crutches to be used as needed during the first week. Typically, no aggressive activity is allowed in the first month and therapy is prescribed for motion if needed. Generally, 3 months is the full recovery time for this type of surgery.
Can a meniscus be repaired?
Yes. Menisci have a poor blood supply and therefore have a poor ability to heal on their own. It is generally felt that if a tear occurs in the outermost third of the meniscus, and attempt should be made to repair the tear. The peripheral third of the meniscus has the capability to heal because this portion has a blood supply. Some surgical centers have attempted to repair more central tears with variable results. Tear pattern (radial tears have poorer results) and patient age (persons over 40 years of age have poorer results) play a role in deciding if a meniscus is repairable. It is felt that formal suture repair is superior to the use of bio-absorbable arrows and darts. There are an increasing number of studies documenting adverse reactions and instances of cartilage damage secondary to ‘proud’ arrow heads. These adverse reactions have caused a decrease in the use of the arrows by the author of the research. If a meniscus is repaired, the recovery process is tailored to allow the meniscus to heal over the course of 8 to 12 weeks.