What is an ankle sprain?
The most common type of ankle injury is a sprain. A sprain is the stretching or tearing of the ligaments around the ankle due to a forceful injury. The most frequently seen sprain is an inversion sprain. This occurs when the ankle is “rolled”, tearing the ligaments on the outside portion of the ankle. Patients often report hearing a “pop” at the time of injury and usually develop pain and swelling on the lateral aspect of the ankle. We will discuss the inversion sprain, as this is by far the most common sprain.
Are there different degrees of sprain?
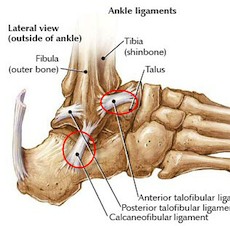
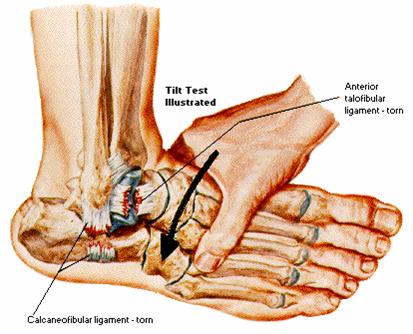
Yes, there is grade I (mild), grade II (moderate), and grade 3 (severe). Three ligaments stabilize the lateral ankle: the anterior talofibular (ATF), calcaneofibular (CF), and posterior talofibular ligaments. In a grade one sprain, the anterior talofibular ligament is stretched causing pain and tenderness just anterior/inferior to the lateral malleolus. There are different definitions to a grade 2 sprain but typically, a grade 2 sprain involves injury to the anterior talofibular and calcaneofibular ligaments. A grade 3 sprain involves the rupture of the ATF and CF ligaments.
How is an ankle sprain diagnosed?
The patient will usually describe a forceful inversion injury. Often they will hear a “pop” and their lateral ankle will swell initially, followed by bruising a few days later. Although uncomfortable, the patient will usually be able to put weight on the ankle, and the inability to do so should make the physician suspicious of a fracture. Examination will involve inspection and palpation of the ankle. Tenderness on the lateral aspect of the ankle anterior to the lateral malleolus indicates an ATF injury. Tenderness below the lateral malleolus indicates a CF injury. Tenderness directly over the lateral malleolus may be indicative of a fracture. A drawer test and tilt test are often performed to assess ankle stability, but these tests are often difficult to interpret. X-rays are usually obtained to rule out a fracture.
What is treatment for an ankle sprain?
The treatment process can be divided into three phases. Modifications to these phases can be made depending upon the severity of the injury. Phase 1 is usually one to two days with the focus primarily on the reduction of inflammation utilizing the principles of RICE (Rest, Ice, Compression and Elevation), Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), and crutches as needed to allow weight bearing as tolerated. Icing should occur 3 times a day, 20 minutes at a time. Phase 2 (2-12 days) focuses on restoration of motion within the ankle complex starting with active range of motion into dorsiflexion and plantar flexion. Inversion and eversion may be too painful to tolerate actively and therefore should be performed either passively or via active-assist. Weight bearing during walking should gradually be increased to allow proprioception (the ability to tell the position of the foot in space) to return and an increase in ankle mobility. Phase 3 (12 days and beyond) should focus on strengthening, agility and endurance. Strengthening should primarily emphasize dorsiflexion and eversion, as these muscles are responsible for resisting inversion-plantar flexion sprains. Proprioception activities can be initiated utilizing a balance board or trampoline. Agility and endurance activities should gradually progress to allow return to functional and athletic activities. Not only do the ligaments need to heal after a sprain, but the nerve endings that have been stretched need to be re-trained to tell the position of the foot in space, thereby preventing recurrence.
Will I need ankle surgery?
Usually, no. Very rarely does someone require surgery for an ankle sprain, and not after a single episode. Occasionally, a patient will develop recurrent instability with incompetent lateral ligaments, which may require reconstruction. This should be fully evaluated with stress x-rays and usually an MRI to evaluate the lateral structures. Also, scar tissue may develop on the lateral aspect of the ankle (lateral gutter) that may require an arthroscopic surgery to clean out.
