What is a SLAP lesion?
 The SLAP (superior labral anterior-posterior) tear is a specific injury to a part of the shoulder joint called the labrum. The shoulder joint is a ball-and-socket joint, similar to the hip; however, the socket of the shoulder joint is extremely shallow, and thus inherently unstable. To compensate for the shallow socket, the shoulder joint has a cuff of cartilage called a labrum that forms a cup for the end of the arm bone (humerus) to move within. This cuff of cartilage makes the shoulder joint much more stable, yet allows for a very wide range of movements (in fact, the range of movements your shoulder can make far exceeds any other joint in the body). A SLAP tear is an injury of this labrum.
The SLAP (superior labral anterior-posterior) tear is a specific injury to a part of the shoulder joint called the labrum. The shoulder joint is a ball-and-socket joint, similar to the hip; however, the socket of the shoulder joint is extremely shallow, and thus inherently unstable. To compensate for the shallow socket, the shoulder joint has a cuff of cartilage called a labrum that forms a cup for the end of the arm bone (humerus) to move within. This cuff of cartilage makes the shoulder joint much more stable, yet allows for a very wide range of movements (in fact, the range of movements your shoulder can make far exceeds any other joint in the body). A SLAP tear is an injury of this labrum.
Various mechanisms of injury have been identified. Some physicians suggested that the lesion was a result of pulling on the biceps tendon during the overhead throwing motion. Others typically felt the injury was sustained due to an acute compression force or traction pull on the shoulder.
What are the signs and symptoms of a SLAP?
Usually people complain of deep anterior pain or a feeling of instability in the shoulder. It is made worse when they put the arm into the “cocked position” ready to throw. Some may complain of pain in the shoulder on lifting heavy objects. A clicking sound and sensation may also be heard when trying to throw.
How is the diagnosis made?
 Physical Examination
Physical Examination
Patients will often point to their pain occurring deep within the shoulder socket- rather than along the side of the arm which is more common in rotator cuff tendonitis. The O’Briens test (see image) is often positive for a deep anterior pain.
MRI
MRI scans are typically used to evaluate the labrum. MRI was 59% sensitive and 85% specific for labral pathology using the arthroscopic examination as the gold standard. Physical examination was 90% sensitive and 85% specific for labral pathology in the same group of patients. By injecting dye (gadolinium) into the shoulder, the accuracy increases for the MRI. The sensitivity of enhanced MRI was 96% compared to 46% sensitivity of unenhanced MRI.
How is a SLAP lesion treated?
Not all SLAP lesions require surgery. Typically, SLAP lesions will not worsen over time. That being said, the deep anterior pain typically will not improve either. If one does not wish to live with these symptoms, surgery is indicated. There are different types of SLAP lesions, and each is treated differently.
A type I tear is repaired by a simple debridement the worn tissue. The surgeon must be sure that the biceps tendon is still securely attached to the labrum.
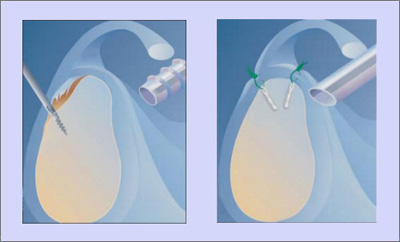
A type II tear involves the biceps tendon and the labrum. The biceps and labrum are becoming detached from their bed on the glenoid fossa. This injury is treated by “tacking” the labrum and biceps complex down to the glenoid with biodegradable suture anchors.
 A type III tear is similar to a bucket handle tear of the meniscus. The labrum/biceps complex is stable on the glenoid but a flap of tissue is hanging down into the joint. This is treated with surgical excision of the flap. There is some debate about repair vs excision; some surgeons will repair if the tear involves 1/3 or more of the labrum.
A type III tear is similar to a bucket handle tear of the meniscus. The labrum/biceps complex is stable on the glenoid but a flap of tissue is hanging down into the joint. This is treated with surgical excision of the flap. There is some debate about repair vs excision; some surgeons will repair if the tear involves 1/3 or more of the labrum.
A type IV tear is complex and involves the labrum and biceps tendon. The labrum presents with a bucket handle type tear that extends into the body of the biceps tendon. The treatment for this complex tear is complex as well. If the biceps tendon/labrum complex is stable on the glenoid, the labral tear will be removed and the biceps tendon repaired. If the complex is unstable on the glenoid the surgeon will use suture anchors to secure the labrum/biceps complex. The biceps tendon will be repaired with suture.
What is surgery like?
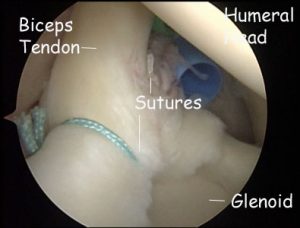
Surgery is usually performed at an outpatient surgery center. The actual surgery takes approximately 90 minutes. You are able to return home approximately 1 to 2 hours after surgery. The operation is performed arthroscopically through 3 small “portals” (5 mm incisions). A portal is placed in the back of the shoulder for the camera. Two portals are placed in the front of the shoulder for the instruments. An anchor (3.5 mm absorbable screw) is inserted into the top of the glenoid (socket). Sutures are then passed on either side of the tear and tied. This re-attaches the labrum to the glenoid.
How is a SLAP repaired?
The anesthesiologist will give you LMA anesthesia. The anesthesiologist uses a mini-tube called a Laryngeal Mask Airway (LMA). This tube is similar to the plastic airway found in a first-aid kit but has a short pipe about the thickness of two of your thumbs and a rubber balloon at the bottom. The balloon holds the tongue out of the way and the short pipe passes the air as you breathe in and out. This LMA is placed after the sedation is given and removed before it is stopped, so you never know you had it at all. Since it is not a full length tube, there is no sore throat.
Surgery is performed in the lateral position. This means that you will be placed on your side.
The operation is performed arthroscopically through 3 small “portals” (5 mm incisions). A portal is placed in the back of the shoulder for the camera. Two portals are placed in the front of the shoulder for the instruments.
An anchor (3.5 mm absorbable screw) is inserted into the top of the glenoid (socket). Sutures are then passed on either side of the tear and tied. This re-attaches the labrum to the glenoid.
SLAP repair
What is it like after surgery?
The actual surgery takes approximately 90 minutes. You are able to return home approximately 1 to 2 hours after surgery. You are placed into a shoulder sling for the first few days. Pain medication and ice are usually required for the first week after surgery. You will return to the office in 7 to 10 days to have the sutures removed. We then begin a course of physical therapy emphasizing motion for the first 6 weeks. Therapy is generally required for 6 to 12 weeks after surgery.
